Shoulder resurfacing & replacement in Burr Ridge
Also serving Plainfield, Morris and surrounding areas
| Procedure | • Outpatient • The ball and socket are replaced with smooth metal and plastic surfaces |
| Duration | 1.5 hours–2 hours |
| Anesthesia | General |
| Recovery | 3–4 months |
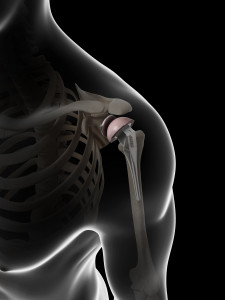
Overview of the Shoulder
The shoulder joint is a ball and socket joint that can wear out in the same fashion as hips and knees. Smooth cartilage surfaces are eventually worn down to bone. The most common diagnosis is Osteoarthritis which causes wear and tear to the joint and loss of smooth motion.

The joint becomes painful and stiff, and activities of daily life are compromised. Shoulder Resurfacing and Replacement are surgical options to restore the normal gliding surfaces of the ball and socket joint.
Shoulder Replacement Procedure Details
Shoulder Resurfacing involves a minimally invasive approach to place a new metallic surface onto the ball of the joint, leaving the natural socket in place if it is not worn out.
Shoulder Replacement involves placement of a metallic surface over the ball of the joint and a smooth plastic surface over the socket of the joint in cases where the socket is also worn.
Surgical treatment is undertaken after thorough history and examination and discussion of all potential options for treatment. This procedure can last from 1.5 to 2.5 hours and usually requires one night in the hospital. Physical therapy after surgery is generally guided by the orthopaedic surgeon with a series of exercises. Return to normal daily activity takes from six to eight weeks.
Arthroscopic Treatment may be an option for certain patients with Arthritis of the shoulder, depending on the severity of the disease. In these cases the treatment is outpatient and may involve removal of bone spurs or shaving of torn cartilage in the joint.
Shoulder Resurfacing & Replacement FAQs
Why Do Patients Have Shoulder Replacement Surgery?
Some of the most common reasons patients require shoulder replacement include:
- Osteoarthritis: This age-related disease gradually wears down the cartilage around joints, allowing bones to rub against each other. The resulting friction can produce inflammation and significant pain.
- Rheumatoid arthritis: This is an autoimmune disease in which the immune system inflames the lining of the joints. The swelling becomes painful and can erode the bone.
- Osteonecrosis: When the flow of blood is obstructed from reaching a portion of bone, the bone tissue can break down and die, causing large joints like the shoulder or hip to collapse.
- Traumatic injury: Patients who suffer a serious injury (such as a sports injury or car accident) may develop arthritis that affects the joint.
- Shoulder replacement revision: If a prior shoulder replacement surgery is misaligned, has healed improperly, or develops complications, it may be necessary to repeat the procedure for better results.
What Are the Benefits of Shoulder Resurfacing?
Shoulder resurfacing has several advantages over traditional shoulder replacement surgery, such as:
- Repairing the shoulder with a less invasive procedure
- Promoting a quicker recovery with less discomfort
- Offering fewer complication risks, with no chance for fat embolus or prosthesis fractures
Unfortunately, not all candidates who need to repair their shoulder joint are suitable for shoulder resurfacing. It is generally limited to patients with mild or moderate cases of arthritis. After assessing apatient’s shoulder, Dr. Burt can provide his professional opinion for the best approach to improve shoulder mobility and diminish pain.

What Is Arthroscopy?
Arthroscopy is a procedure that allows Dr. Burt to diagnose and treat shoulder (or other joint) problems when an X-ray does not provide a complete picture. Instead of making a large incision to assess the shoulder, he makes a tiny incision through which he inserts a small camera that transmits a high-quality video to an external monitor.
Dr. Burt can also use arthroscopy (rather than a more invasive surgery) to address issues like:
- Torn cartilage or ligaments
- Inflammation or scarring on the shoulder joint
- Loose bone fragments
What Activities Should Patients Avoid After Shoulder Replacement?

Although patients’ activities are restricted for a couple months while recovering from shoulder replacement, they should be able to resume normal activities and use of the involved arm thereafter. For long-lasting results, patients should not overexert or overuse the surgical arm, which can wear down and compromise the life of the artificial joint. Consult with a physician before:
- Lifting extremely heavy weights or objects
- Participating in high-impact sports that utilize arm and shoulder force, like boxing
- Hammering or performing other repetitive arm and shoulder movements
When Is a Patient Too Old (or Too Young) for Shoulder Replacement?

Most patients who undergo shoulder replacement are in their 60s or 70s due to aging’s effects on the joints, but there is not a formal age limit for patients who remain a good candidate for the surgery. Many of the patients who have shoulder replacement at a younger age require surgery because of a sports injury.
Because shoulder replacements can eventually wear out, some younger patients decide to postpone surgery. Ultimately, the timing of the surgery is usually dictated by the amount of physical discomfort the patient is experiencing. While a patient who has shoulder replacement in his or her 40s is more likely to require a revision surgery a couple decades later, that is preferable to grappling with shoulder pain each day.
What Is the Difference Between Shoulder Resurfacing and Full Replacement?
Shoulder resurfacing and total shoulder replacement are both surgical treatments for joint damage, but they differ in how much of the joint is replaced.
- Shoulder resurfacing involves capping the humeral head (the ball of the shoulder) with a metal implant without replacing the socket.
- Full shoulder replacement involves replacing both the ball and the socket with artificial components.
- Resurfacing typically preserves more bone, making it an appealing option for younger or more active patients.
- Recovery may be faster with resurfacing due to the less extensive nature of the surgery.
- Full replacement is often preferred when joint damage is advanced or both sides of the joint are compromised.
How Long Do Shoulder Replacements Typically Last?
Modern shoulder prostheses are designed to be durable and long-lasting.
- Most total shoulder replacements last 10 to 20 years or longer.
- Longevity depends on factors like implant type, surgical technique, and patient activity level.
- Patients who avoid high-impact or repetitive overhead activities may extend the life of their implant.
- Follow-up appointments help monitor implant function and detect wear or loosening early.
- Revision surgery is possible if components wear out over time.
What Is the Average Recovery Time after Shoulder Surgery?
Recovery time varies depending on the extent of surgery and patient health, but most patients can expect a staged timeline.
- Hospital stays are typically one to two days for full replacement.
- Sling use is usually required for 2–6 weeks postoperatively.
- Physical therapy often begins shortly after surgery and continues for several months.
- Most patients return to normal daily activities within 3 months.
- Full recovery, including strength and range of motion, may take 6–12 months.
Are There Risks Associated with Shoulder Replacement Surgery?
All surgeries carry risks, but complications with shoulder replacement are relatively uncommon.
- Potential risks include infection, blood clots, nerve injury, or implant loosening.
- Stiffness or continued pain can occur if rehabilitation is not followed properly.
- Proper surgical technique and patient compliance with post-op instructions help minimize risk.
- Dr. Burt carefully evaluates each patient to ensure safety and optimal outcomes.
Will I Need Physical Therapy after Shoulder Surgery?
Yes, physical therapy is a critical part of the recovery process.
- Therapy helps restore range of motion and rebuild shoulder strength.
- It typically begins within a few days post-surgery under medical supervision.
- Exercises progress over many weeks to gradually improve function and endurance.
- Consistent participation significantly influences long-term success.
- Physical therapy protocols are customized for resurfacing vs. full replacement patients.
Does Insurance Typically Cover Shoulder Replacement Procedures?
Yes, most health insurance plans provide coverage for shoulder replacement when deemed medically necessary.
- Coverage often includes pre-surgical evaluations, imaging, surgery, anesthesia, and post-op therapy.
- Prior authorization from the insurance provider may be required before surgery.
- Out-of-pocket costs vary depending on the plan, deductible, and provider network.
- Patients are encouraged to contact their insurance company and the surgical coordinator for a detailed estimate and pre-approval process.
How does Dr. Burt Determine the Best Treatment Plan?
Dr. Burt uses a personalized and evidence-based approach to create optimal treatment plans.
- He conducts a thorough physical exam and reviews detailed imaging such as X-rays or MRIs.
- Patient goals, age, activity level, and severity of joint damage are carefully considered.
- When possible, joint-preserving options like resurfacing or arthroscopy are explored first.
- In cases of advanced degeneration, full replacement may offer the most effective solution.
- Dr. Burt prioritizes long-term function and minimizing future complications.
Schedule an Appointment Today
Over the years, Dr. David Burt has helped many patients suffering from shoulder injuries regain their active lifestyles and live pain free. In addition to treating arthritis, Dr. Burt offers rotator cuff surgery, labrum tear treatments and shoulder dislocations surgery. To schedule a consultation at Midwest Sports Medicine Institute, call our Burr Ridge office at (630) 455-2000, our Plainfield office at (815) 267-8825, or our Morris office at (815) 941-1885.
Recent posts
Lateral Decubitus Position for Arthroscopic Suprapectoral Biceps Tenodesis

The purpose of this report is to describe arthroscopic suprapectoral biceps tenodesis in the lateral decubitus position. Many technique descriptions for this procedure emphasize the beach-chair position to obtain optimal anterior subdeltoid visualization of the relevant anatomy. This is not...
Read MorePhysician's corner: Dr. David Burt

Two years ago, Dr. David Burt opened up his third clinic with Midwest Sports Medicine Institute in Burr Ridge. Along with locations in Plainfield and Morris, Dr. Burt is able to treat countless of athletes of all ages and levels...
Read More
